
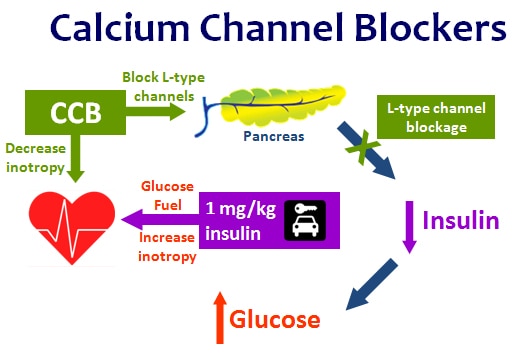
If the fluid overload is a concern, the insulin can be concentrated to 10 U/mL.Dextrose: 0.5 g/kg/hr (titrate to maintain glucose 110 – 150 mg/dL.Regular insulin: start 0.5 – 1 unit/kg/hr.If serum glucose Intravenous bolus of regular insulin at a dose of 1 unit/kg.Hyperinsulinemia Euglycemia Therapy (HIET) Initiation:.Using Hyperinsulinemia Euglycemia Therapy(Lugassy 2015) Even in a CCB poisoned animal model insulin increases myocardial glucose uptake resulting in improved contractility.In vitro and in vivo evidence has shown insulin’s positive inotropic and chronotropic effects( Reikeras 1985, Kline 1995).In a stressed state the heart turns to prefer carbohydrate and insulin appears to facilitate this preference.
Beta blocker antidote glucagon moa free#
Under normal physiologic conditions the heart prefers to use free fatty acids as its primary energy source.CCB inhibits lactate oxidation resulting in lactic acidosis.As a result of lower insulin levels, glucose cannot move into the myocardial cells at a rate sufficient to respond to demand. CCB inhibits insulin secretion from the beta-islet cells of the pancreas.Blockade of calcium channels leads to effects outside the cardiovascular system as well.The liver responds to this increased demand by releasing glucose via gluconeogenesis, ultimately resulting in hyperglycemia. As the myocardium becomes stressed, it switches from catabolizing free fatty acids to catabolizing carbohydrates.This can lead to vasodilation, decreased systemic vascular resistance, bradycardia, conduction delay, decreased contractility, hypotension and cardiogenic shock. BBs and CCBs lead to decreased intracellular calcium within the myocardial cells.Calcium channel blocker overdose is less frequent than that of beta-blockers, but has been associated with the highest mortality rates among the cardiovascular drug overdoses( Woodward 2014).In 2012 alone, there were 24,465 beta-blocker exposures (Mowry 2013). The most common cause of poison-induced cardiogenic shock is beta-blocker toxicity.Cardiogenic shock due to beta-blocker (BB) or calcium channel blocker (CCB) toxicity is frequent and potentially lethal.For cases of CCB poisoning where cardiotoxicity is evident, a combination of calcium and epinephrine should be used initially, reserving HDIDK for refractory cases. For cases of beta-blocker poisoning where symptomatic bradycardia and hypotension are present, high-dose glucagon is considered the first-line antidote. Poisoning by beta-blockers or CCBs usually produces hypotension and bradycardia, which may be refractory to standard resuscitation measures. Health-system pharmacists should be aware that when these drugs are used as antidotes, higher than normal dosing is needed. For cases of CCB poisoning where cardiotoxicity is evident, first-line therapy is a combination of calcium and epinephrine high-dose insulin with supplemental dextrose and potassium therapy (HDIDK) is reserved for refractory cases. Traditionally, antidotes for CCB overdose have included calcium, glucagon, adrenergic drugs, and amrinone. However, in beta-blocker poisoning where symptomatic bradycardia and hypotension are present, high-dose glucagon is considered the first-line antidote. Therapies include beta-agonists, glucagon, and phosphodiesterase inhibitors. Poisoning by CCBs is characterized by cardiovascular toxicity with hypotension and conduction disturbances, including sinus bradycardia and varying degrees of atrioventricular block. The common feature of beta-blocker toxicity is excessive blockade of the beta-receptors resulting in bradycardia and hypotension. In overdose, beta-blockers and CCBs have similar presentation and treatment overlaps and are often refractory to standard resuscitation measures. Beta-blockers and CCBs represent the most important classes of cardiovascular drugs.
Overdoses with cardiovascular drugs are associated with significant morbidity and mortality. The toxic effects and treatment of beta-adrenergic blocker and calcium-channel blocker (CCB) overdose are reviewed.


 0 kommentar(er)
0 kommentar(er)
